The ACHP Difference
Driving access and affordability
Throughout 2022, ACHP worked closely with its member companies and remained focused on ensuring adults and children in communities across the country gained and maintained affordable, high-value health coverage and care.
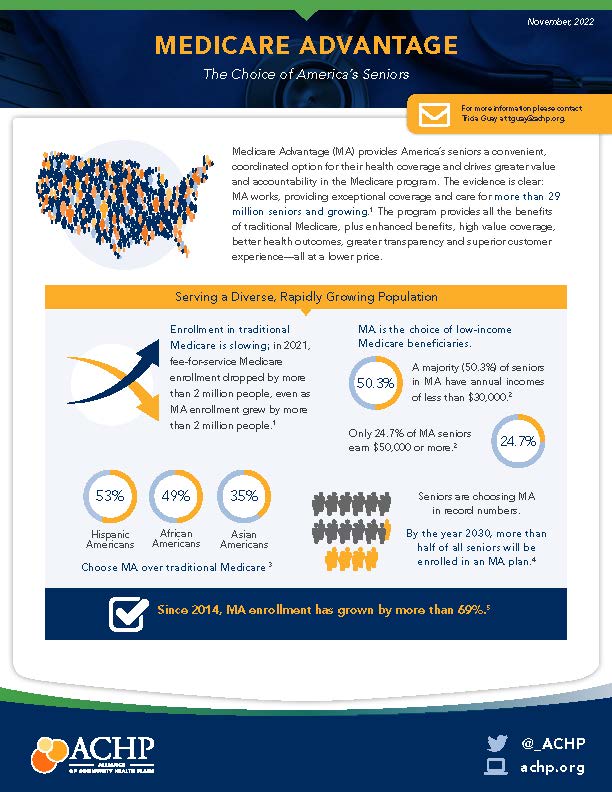
- Provided critical information that led to a Senate Finance Committee investigation and report about inappropriate and misleading Medicare Advantage (MA) marketing abuses. Following the report’s publication, CMS announced it will increase oversight of aggressive marketing behaviors.
- Extended enhanced ACA tax credits for three years – through 2025 – ensuring millions of Americans will maintain access to quality, affordable health coverage.
- Remained the only national payer organization to push Congress and the Administration for comprehensive drug pricing reform.
- Lobbied successfully for the passage of the Inflation Reduction Act (IRA), a “win for consumers.”
- Aggressively pushed the Biden Administration to limit coverage of controversial drug Aduhelm to Medicare beneficiaries participating in clinical trials.
- Limiting coverage of Aduhelm led to the largest decrease in Medicare Part B premiums in a decade. Monthly premiums will drop 3.1% in 2023.
- Successfully advocated to protect the MA program and received an 8.5% MA rate bump in the 2023 Rate Notice.
- Worked with the Biden Administration to shape over-the-counter COVID testing requirements, ensuring equitable and affordable access to life-saving tests.
- Shaped end-of-year spending bill, which included key ACHP priorities, such as:
- Extensions on: the Acute Hospital Care at Home waiver; telehealth flexibilities tied to the public health emergency including a delay of the in-person requirement to receive telemental health care; and enhanced Medicaid payments for states that meet reporting requirements
- 12 months of continuous coverage for children in Medicaid and CHIP
- Flexibility for states to provide up to 12 months of post-partum coverage.
Differentiating through quality
Consistently recognized as leaders in providing top-quality and high-value care, ACHP members emphasize the importance of their unique payer-provider models and commitment to the communities in which they operate.
- Despite providing fewer than 10 percent of MA contracts nationwide, ACHP members represent one-third of all 5-star contracts, with 18 ACHP members having at least one contract that earned at least 4 stars.
Giving voice to nonprofit community health plans
ACHP elevated the collective voice and strength of its membership seeking to influence key decisionmakers and build political support for policies that enable its members to care for their communities.
- Participated in the first White House Conference on Hunger, Nutrition and Health in 50 years, supporting ACHP’s food security framework recommendations.
- Hosted the first in-person ACHP Symposium since 2019, welcoming a record 179 attendees, including Administration officials, members of Congress and swimming legend Diana Nyad.
- Convened more than 100 attendees from ACHP member plans at the Spring Summit in Chicago for discussions about improving health equity, the future of digital health, trust in health care and adapting to a post-COVID landscape.
- Hosted ACHP members in Washington for a Policy and Advocacy Strategy Summit to prepare for a new divided government in 2023.
- Appealed to Congress via a STAT News op-ed authored by Ceci Connolly and Kaiser Permanente’s Stephen Parodi regarding hospital-care-at-home extensions beyond the PHE.
- Spotlighted three ACHP plans that expanded acute-care-at-home services to reach at-risk, rural seniors in a Becker’s Payer Issues op-ed by Ceci Connolly.
- Amplified ACHP’s messaging in a cnn.com op-ed by Dr. Jennifer Lee on the need to address Medicaid redeterminations as the PHE winds down.
- Secured 150+ media mentions, including The New York Times, The Wall Street Journal, Modern Healthcare, STAT News and TIME.



Ceci Connolly
ACHP President & CEO
quoted in Modern Healthcare

Dr. Jennifer Lee
ACHP Chief Medical Officer
CNN op-ed






Bringing members together
Executives of its member plans look to ACHP to foster peer-to-peer networking via task forces, work groups and virtual communities. This year, ACHP launched six new groups:
- ACHP Executive Council: Comprised of strategic leaders from member companies, the council shapes ACHP differentiation initiatives and related policy proposals. Overall, ACHP members report the following marketplace differentiators:
- Greater decreases in silver-plan premiums
- Higher Net Promoter Scores
- Higher member retention rates
- Greater use of price transparency tools
- MA Tiger Team: A visionary effort to develop Next Gen MA proposals.
- Health Equity Community: Convening health equity leaders to network, share best practices feedback on policy proposals.
- Drug Pricing 2.0 Work Group: Addressing current IRA implementation concerns and setting future industry priorities.
- ePrior Authorization and Price Transparency Task Force: Focused on ePrior Authorization, CMS Advanced Explanation of Benefits and Good Faith Estimate for Covered Individuals.
- Medicaid Work Group: Intel exchange on topics such as redeterminations, contract procurement and strategies to address social determinants of health.
Remaining committed to health equity
ACHP and its members remain committed to making access to high-value health care and treatment plans – and the ensuing outcomes – equitable for all members of the communities they serve.
- ACHP's Maternal Health Task Force shared insights from members with the Robert Wood Johnson Foundation’s Raising the Bar Project. The initial project led to a grant extension on how health plans can play a greater role in improving maternal health outcomes and equity.
- ACHP’s Ceci Connolly interviewed Sue Turney, M.D., CEO of Marshfield Clinic Health System, on the Her Story podcast to discuss prioritizing diversity in the health care workforce.
- ACHP’s Health Equity Community exchanged intel at its inaugural meeting on strategies to address health disparities, including ways to implement ACHP’s health equity framework.
- ACHP’s internal Education, Training and Staff Conversations Task Force hosted a series of gatherings that increased awareness of the diversity of backgrounds and experiences each of us bring to our work every day. Conversations covered topics including:
- Pronouns and Inclusivity
- Disability and Ableism
- Food Justice
- Hispanic Heritage and Diversity in the Workplace

Transforming health care delivery
ACHP brings industry leaders together to share best practices focused on outcomes, quality benchmarks and value delivery to their communities.
- Published two new case studies, featuring Baylor Scott & White Health Plan and Security Health Plan, focused on expanding virtual care to ensure beneficiaries maintain access to vital health care services.
- Hosted a webinar on the launch of the new 988 crisis number.
- ACHP’s Ceci Connolly interviewed Dr. Mandy Cohen, former North Carolina Secretary of Health and current CEO of Aledade Care Solutions, on the Healthy Dialogue podcast to discuss value-based care.
- Led a panel of ACHP member company executives at AcademyHealth’s National Health Policy Conference, discussing using telehealth to address long-standing mental health inequities.
- Participated in “Hospital-At-Home: How Payers are Driving Patient-Centered Care Anywhere” at the American Telemedicine Association’s 2022 conference, with Ceci Connolly and representatives from SelectHealth/Intermountain, Kaiser Permanente and Marshfield/Security Health Plan.
- Participated in Politico Health Care Summit, “Cracking America’s Health Care Access Puzzle,” featuring Ceci Connolly.
- Participated in thINc 360, the Healthcare Innovation Congress, featuring Ceci Conolly’s keynote on “Policy Changes and Reform: What’s Ahead?” and Dr. Jennifer Lee moderating the “Path to Improving Outcomes and Optimizing Care for Medicaid Beneficiaries,” with representatives from HealthPartners and Intermountain.
- Participated in Becker’s Healthcare Payer Issues roundtable, featuring Ceci Connolly and Kaiser Permanente on “Top Priorities for Payer Executives Today,” as well as representatives from Presbyterian Health Plan, Priority Health and Group Health Cooperative of South Central Wisconsin.
Enhancing market competitiveness
Proprietary data tools and analytics enable ACHP to tell compelling stories that differentiate its members’ plans, always with a focus on improving community health via community-oriented solutions.
- Launched a new Utilization Benchmarking tool, a highly interactive report that allows users to benchmark their respective plan utilization performance against other national, state and ACHP plans.
- Facilitated a deep dive with ACHP’s chief executives and external thought leaders at the Annual CEO Summit regarding cutting-edge topics, challenges and opportunities for ACHP member companies to differentiate themselves.
- Launched a cloud-based member vendor inventory as a robust digital resource for vendor information and recommendations as a platform for alignment around vendor strategies.